Abstract

Introduction: Non-alcoholic fatty liver disease (NAFLD) is the most common cause of chronic liver disease. Studies have shown a strong association between NASH (non-alcoholic steatohepatitis) cirrhosis and portal vein thrombosis (PVT). Data is scarce on the association of NASH and venous thromboembolism (VTE), with one such study predicting a 2.5-fold increased risk for VTE in comparison to other liver diseases in hospitalized patients. The mechanism is believed to be hepatocellular injury causing a chronic inflammatory state leading to unregulated activation of procoagulant factors. There is no prior analysis of the degree of steatosis and fibrosis (measured on transient elastography, commonly known as Fibroscan®) in NASH patients and its association with VTE. We performed an analysis to study the risk of unexplained VTE in patients with NASH.
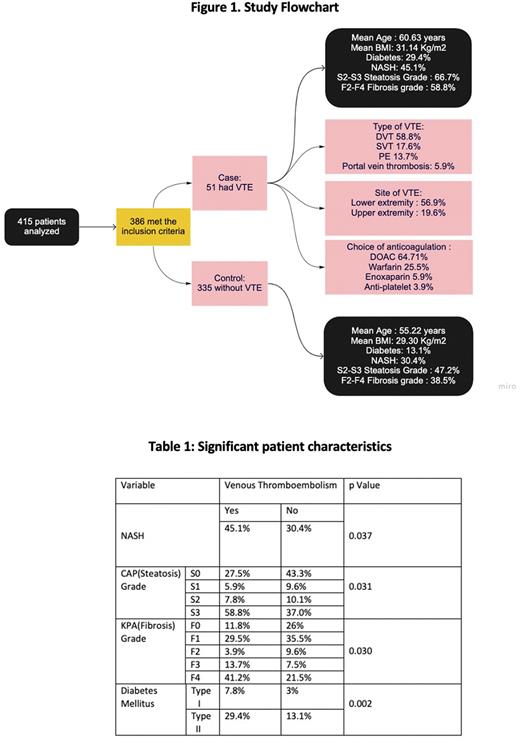
Methods: In our case-control study, we included patients with a documented diagnosis of NASH and excluded patients with inherited thrombophilia, hemoglobinopathy, malignancy, alcohol use disorder, autoimmune hepatitis, and primary biliary cirrhosis. Collected data included age, tobacco use, recreational drug use, medical history, and vibration-controlled transient elastography (VCTE) scores. Venous thromboembolism specific data included location, type of anticoagulant, need for hospital stay, and history of VTE recurrence. Steatosis was categorized as S0-S1 (mild) and S2-S3 (moderate to severe) based on the controlled attenuation parameter (CAP) score. Fibrosis was classified based on the kilopascal(KPA) score and graded as F0-F1 (metavir stage), F2, F3, and F4(cirrhosis). Chi-square and Mann-Whitney U tests were used for qualitative and quantitative variable analysis, respectively. Furthermore, we computed logistic regression using VTE as a dependent variable.
Results: A total of 415 patients were analyzed, and 386 met the inclusion criteria (Figure 1). Fifty-one patients were in the VTE group and 335 in the non-VTE group. Patients with VTE had a mean age of 60.63 years compared to 55.22 years in the non-VTE group (p=0.014). Patients with VTE had a higher body mass index (31.14 kg/m² vs. 29.30 kg/m²) and a higher prevalence of diabetes mellitus (29.4% vs. 13.1%, p=0.002). The history of NASH was significantly higher in the VTE group (45.1% vs. 30.4%, p=0.037). Further, moderate to severe steatosis was significantly higher in the VTE group (66.7% vs. 47.2%, p=0.009). Similarly, the F2-F4 fibrosis grade had a higher prevalence of 58.8 % in the VTE group compared to 38.5% in the non-VTE group (p=0.006) (Table 1). On logistic regression, using VTE as a dependent variable, diabetes mellitus type II had an OR =1.702 (p = 0.015) and F2-F4 fibrosis grade had an OR = 2.5 (p=0.033).
In the VTE group, 58.8% had deep vein thrombosis (DVT), 17.6 % had superficial venous thrombosis (SVT), 13.7 % had pulmonary embolism (PE), 5.9% had portal vein thrombosis, and embolic stroke (3.9%). The most common location of VTE was the lower extremity (56.9%), followed by the upper extremity (19.6%). Right-sided VTE (66.7%) was more common and a majority of patients (74.5%) required hospital admission with 2% requiring ICU admission. Concerning anticoagulation 64.71% of patients were on direct oral anticoagulants (DOAC), 25.5% were on warfarin, and 84.3% of patients continued indefinite anticoagulation.
Discussion: Our analysis shows that NASH is an independent risk factor for VTE, especially DVT. Demographics including gender, tobacco use, alcohol consumption, and ethnicity, were equally distributed between the two groups. There is a statistically significant association between the incidence of VTE and moderate to severe steatosis and fibrosis. The current management strategy for NASH includes abstinence from alcohol and intense lifestyle modification to lose weight. Newer medications like glucagon-like peptides (semaglutide) and bariatric surgery are other recommended modalities for weight loss. All hospitalized patients should be considered for medical thromboprophylaxis, particularly in those with NASH, where a high index of suspicion for VTE should be maintained even in the presence of thromboprophylaxis. Additional studies are needed to analyze the risk of bleeding in this patient population who continue indefinite anticoagulation. Another area of interest would be to determine the reversibility of VTE risk with appropriate management of NAFLD.
Disclosures
No relevant conflicts of interest to declare.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal